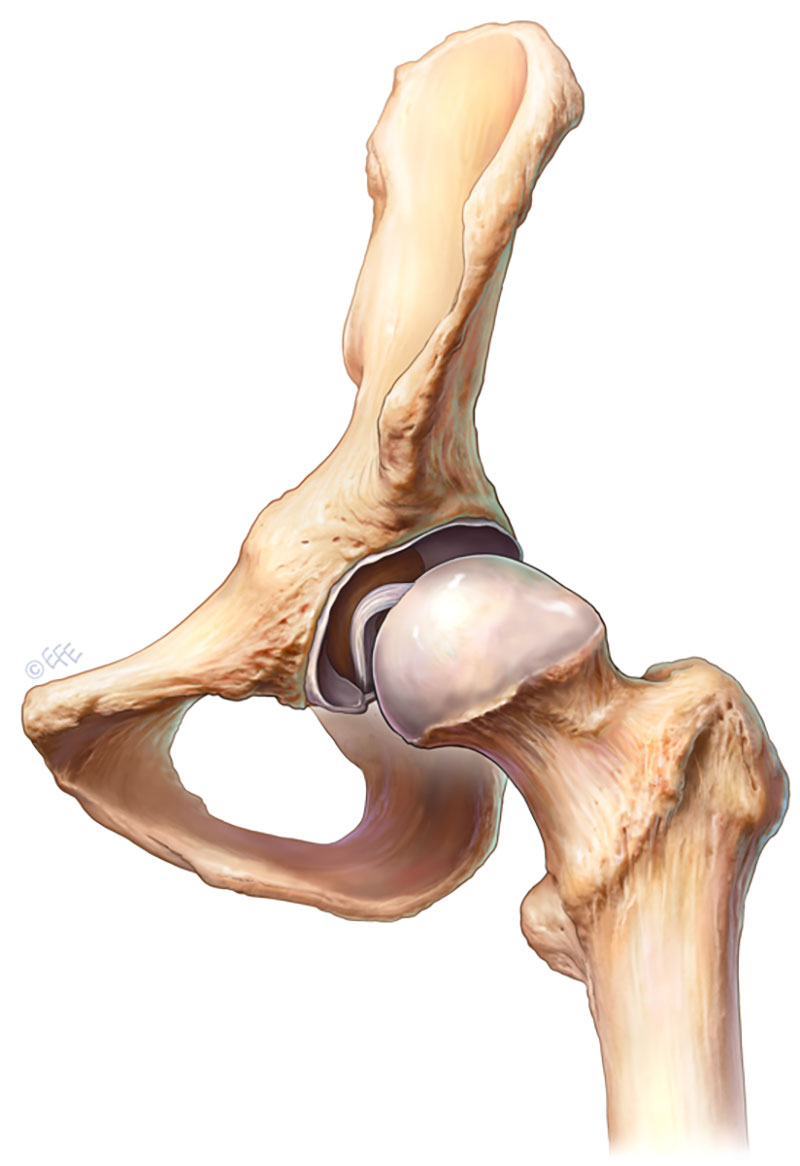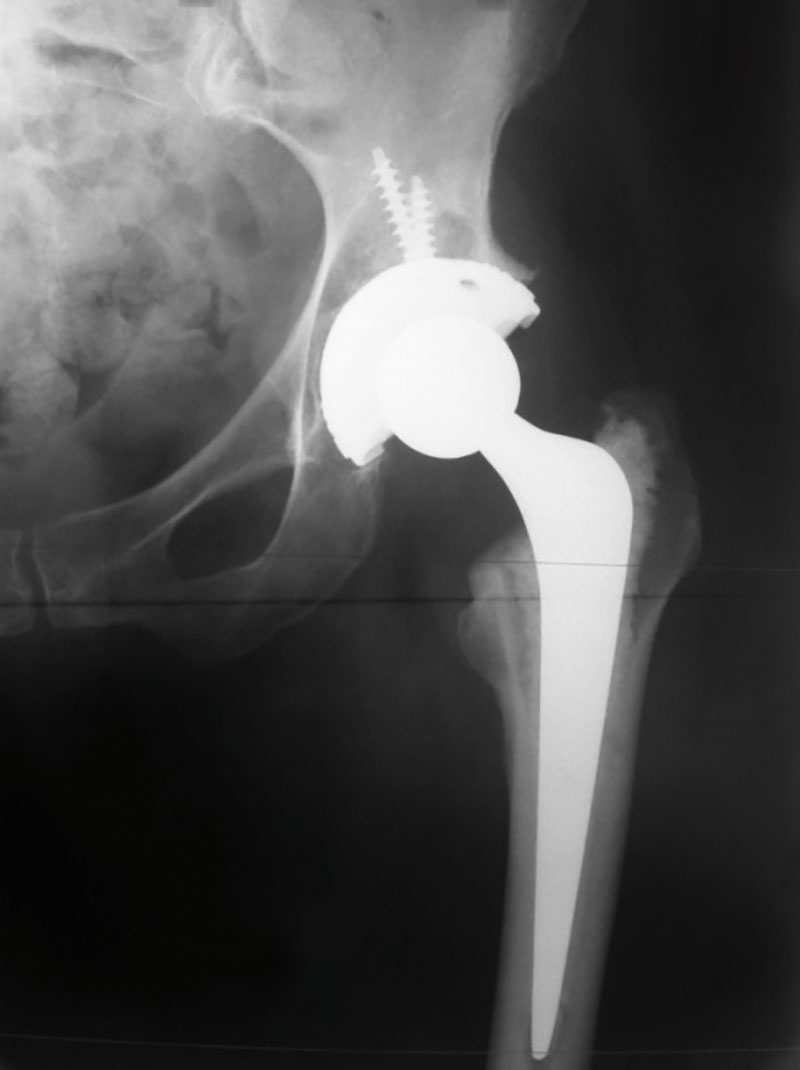
(Figure 1. Cartilage damage seen in Osteoarthritis)
Arthritis of the hip joint is a common condition. It usually affects middle age and older people resulting in over 40,000 hip replacements being performed in Australia per year to relieve sufferers of their pain. It comes about when the cartilage which overlies the femur (leg) bone or lines the acetabulum (pelvic) bone wears out and exposes “bone on bone” articulation resulting in pain, stiffness and disability.
Many forms of arthritis have been described. Osteoarthritis is the most common form characterized by the break-down of the joint’s cartilage. The exact cause of osteoarthritis is unknown but it may occur in families (genetic predisposition), post injury or as a result of infection in the joint.
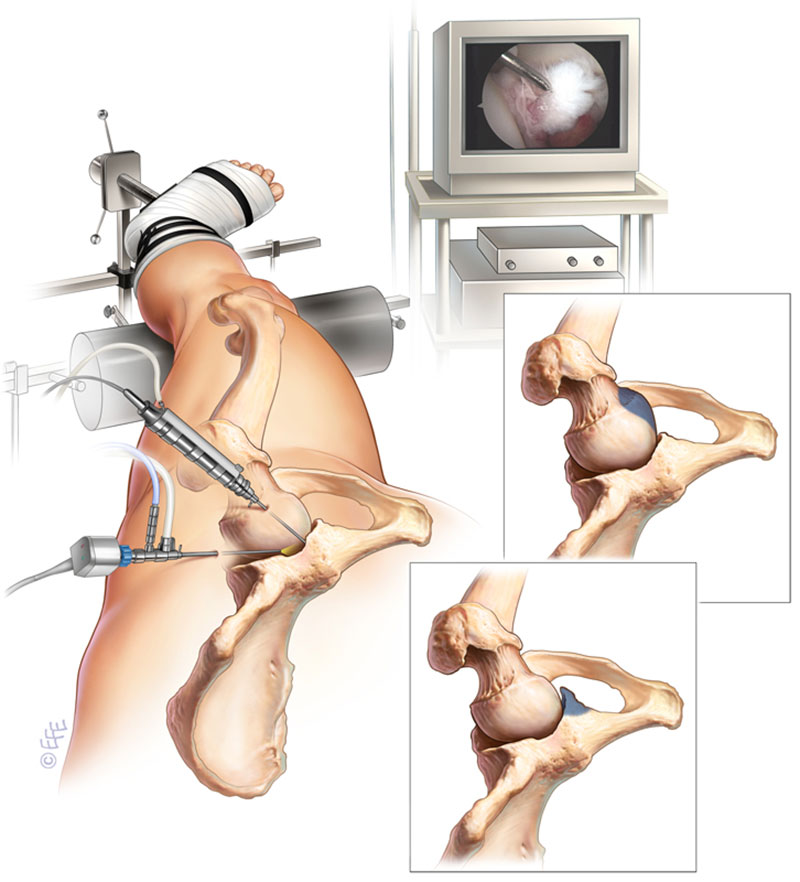
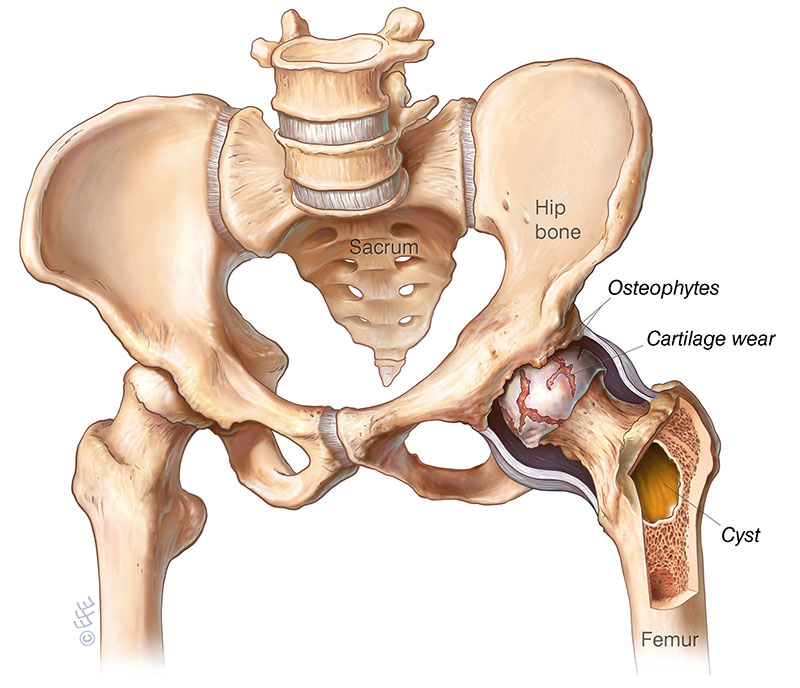
(Figure 2. Severe Osteoarthritis of the left hip)
The next most common form of arthritis is known as rheumatoid arthritis. This is a chronic inflammatory disease of the joint and soft tissues often resulting in the rapid onset of pain, swelling and stiffness with marked joint destruction. Rheumatoid arthritis is more common in women, and is caused by the body’s own immune system attacking the joints, often affecting the small joints of the body first i.e. those of the hands and fingers before involving the larger lower limb joints.
Other forms of arthritis are less common and broadly categorized into the term “inflammatory arthritis” including such conditions as ankylosing spondylitis, systemic lupus erythematosus (SLE), gout and juvenile arthritis.
Arthritis of the hip joint often has an insidious onset characterized by groin, lateral thigh or less commonly buttock pain which may radiate down the leg to the knee and beyond. The pain is worse with activity, limits walking distance and often will cause disturbance of sleep. Early morning stiffness is a common symptom and increases as the disease progresses, often resulting in the inability to reach down to put on ones socks and shoes.
The diagnosis of arthritis is usually made on the basis of the symptom pattern, stiffness and irritability of the joint along with X-ray changes.
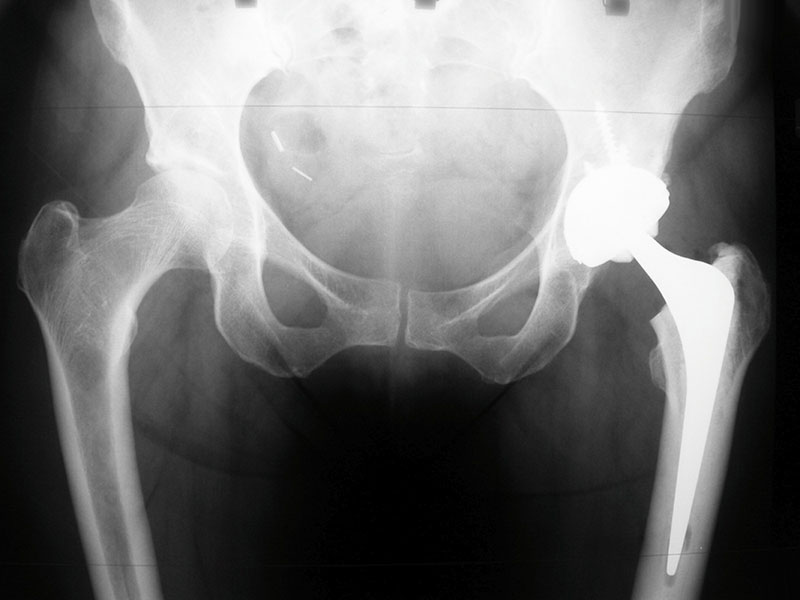
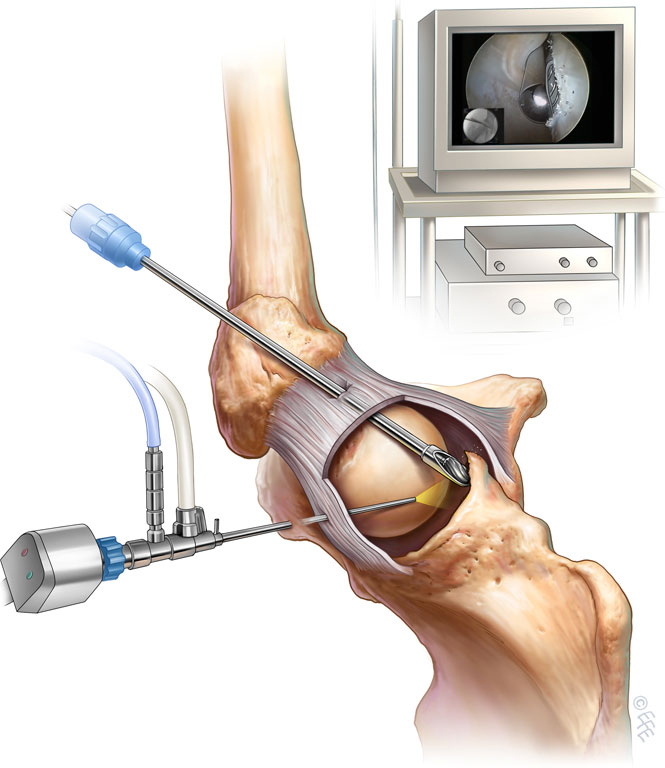
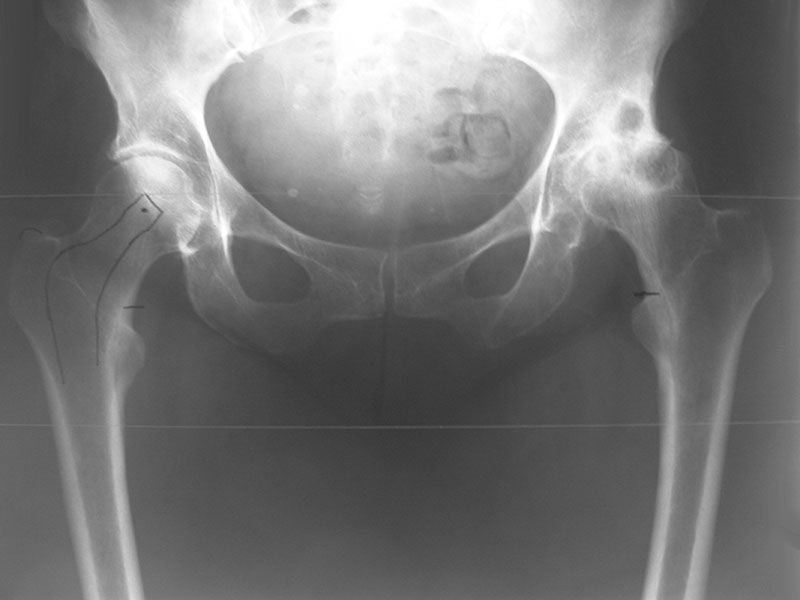
(Figure 3. Left total Hip replacement)
The early management of arthritis involves non-surgical modalities. These include a modification of activities to avoid the aggravating factors e.g. cessation of running / jumping pursuits and substituting those with more suitable activities e.g. walking, cycling or swimming. Weight optimization and the cessation of smoking will increase the lifespan of the remaining cartilage as can dietary supplementation with glucosamines and fish oils. Simple analgesia in the form of paracetamol combined with anti-inflammatory medication is first line pain control. Physiotherapy and hydrotherapy are used to strengthen the muscles surrounding the joint and walking aids in the form of a stick or frame can make ambulation safer and less painful. A walking stick should be held in the opposite hand to the hip that is affected.
When these first line measures for managing the pain from your arthritic hip fail to provide effective relief then it may be time to consider hip replacement surgery.